Prioritize the need and make a positive impact
Predicting, planning, and adjusting staffing decisions
Generally, unit-based schedules are developed weeks in advance and are based on averages. A unit’s person- nel budget and staffing plan (schedule) are developed according to how it measures workload (most organizations use hours per patient day) and its average daily census.
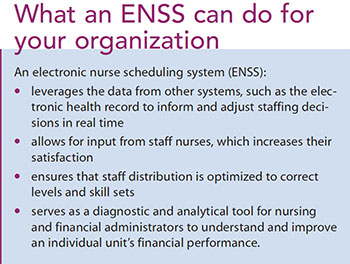
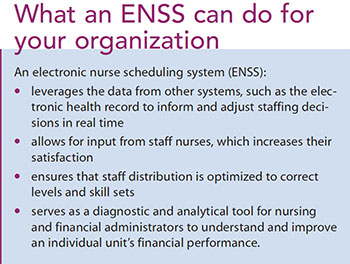
Staffing, however, is done in the moment and is informed by the current patient demand, including census, acuity, and predicted shift turbulence (admissions, transfers, and discharges). All of these variables can change rapidly and either increase or decrease the personnel needs for that shift. In addition, units will experience sick calls and other disruptions to their normal staffing patterns, often with limited notice. As both patient factors and resources change, staffing adjustments must be made across the organization to provide appropriate staffing levels in all clinical areas. An ENSS that’s updated in real time can provide the information needed to inform and enhance staffing decisions when unexpected changes occur.
For example, a supplemental staffing RN trained to float to multiple areas, or other RNs with a specific set of competencies, may be available and agreeable to reassignment. But without a system that can identify their availability, that information might go unknown.
Alternative solutions may be possible, but frequently they come with trade-offs to quality, morale, or finances. For instance, floating unit-based or inexperienced nurses outside their area of competency may adversely affect care delivery and decrease job satisfaction and morale. Permitting the use of overtime may provide another quick solution, but will have a negative financial impact to the operating budget and increase the risk of errors in judgment that can occur when working an excessive number of hours. Eventually, consistent overtime can lead to team burnout and turnover.
An ENSS can alleviate some of these issues by quickly helping managers find staff members with the time and skill set required. The ENSS provides immediate visibility to the data needed for staffing decisions that benefit both the patient and staff. Patients receive the care they need, and nurses see more consistent logic to the changes in their daily routine.
Increasing staff input and ensuring optimized staff distribution
Many nursing organizations, including the American Nurses Association and the American Nurses Credentialing Center (as part of its Magnet Recognition® program), recommend unit-level staff involvement in scheduling and staffing. More importantly, nurses overwhelmingly voice the importance of having input into their personal schedules as well as organizational staffing and scheduling policies.
The ENSS provides fair access to staffing and scheduling processes for all unit staff and takes a systematic approach to ensure appropriate distribution of nurses ensure that charge nurses are scheduled appropriately for all shifts and full-time nurses are working their full commitment of weekends and nights. More importantly, it can help managers keep track of the number of hours a nurse is working to ensure he or she isn’t working too much.
The system can be tailored to reflect unit and organizational policies that have been agreed upon by unit-based staff, increasing perceptions of fairness, accountability, and adherence to union work rules. And because staff interact directly with the system, managerial oversight is minimized, decreasing the amount of time that unit leaders spend managing the schedule. Some organizations even allow self-directed floating, which not only saves administrative time, but also increases nurses’ satisfaction when they have a say in the time and location of their shift.
Overall, this level of staffing control leads to higher retention rates, a statistic that benefits both quality and costs. Satisfaction with staffing is measured on the Magnet surveys and is often a part of employee surveys because of the correlation of staff satisfaction with staffing, quality, and turnover outcomes. ENSS’s capability for nurses to interact directly with the system in real time creates active involvement with their schedules and staffing opportunities, increasing their chance to be satisfied with those changes.
Improving unit financial performance
Because a unit’s personnel budget and staffing plan are inherently linked, the data needed to effectively manage a unit’s financial performance are embedded in an ENSS. The staffing plan should be built on the resources allocated in the personnel budget and account for a mix of staff and nonproductive and nonworked hours.
The ENSS uses the unit staffing plan as the foundation for creating the schedule, and then tracks in real time the unit’s ability to effectively execute that plan. Unit financial success depends on its ability to determine when additional resources are warranted and justifiable and to identify opportunities to reallocate resources based on decreased patient workload; in essence, a budget versus actual adjusted comparison. This comparison can trigger nurse leaders and financial ad- ministrators to act when short and long-term interventions are needed to improve unit financial performance.
For example, if the need to extend orientation for a new employee results in excess nursing worked hours, this short-term expense may be justifiable and can be easily tracked in the ENSS. If, however, a unit is struggling with a highly variable census that creates issues with matching resources and workload, this will be evident in the scheduling system and allow the team to create mitigation strategies. In addition, the system can note seasonal acuity and census variations to provide predictive forecasting when looking at long-term scheduling adjustments.
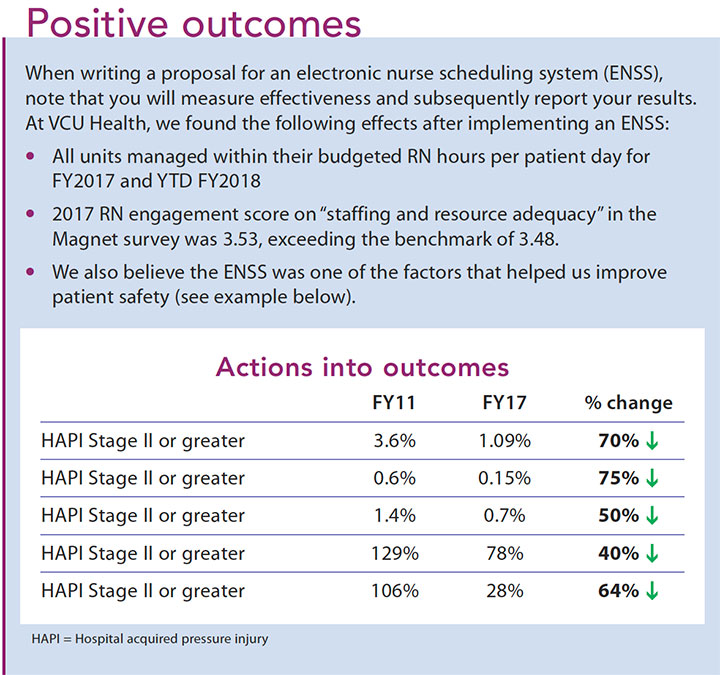
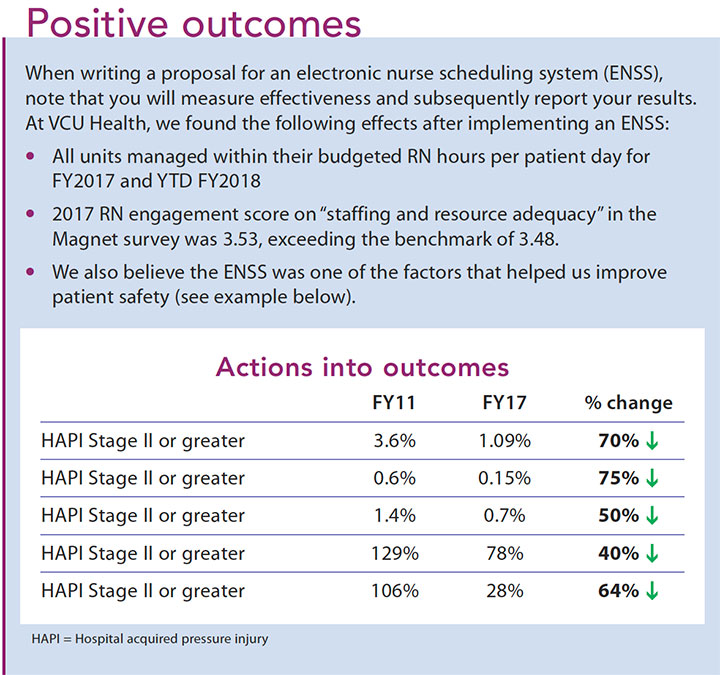
All of these advantages work together to allow managers and administrators to investigate and solve operational issues faster, making them better financial stewards of their operating budget. (See Positive outcomes.)
Prioritizing the investment
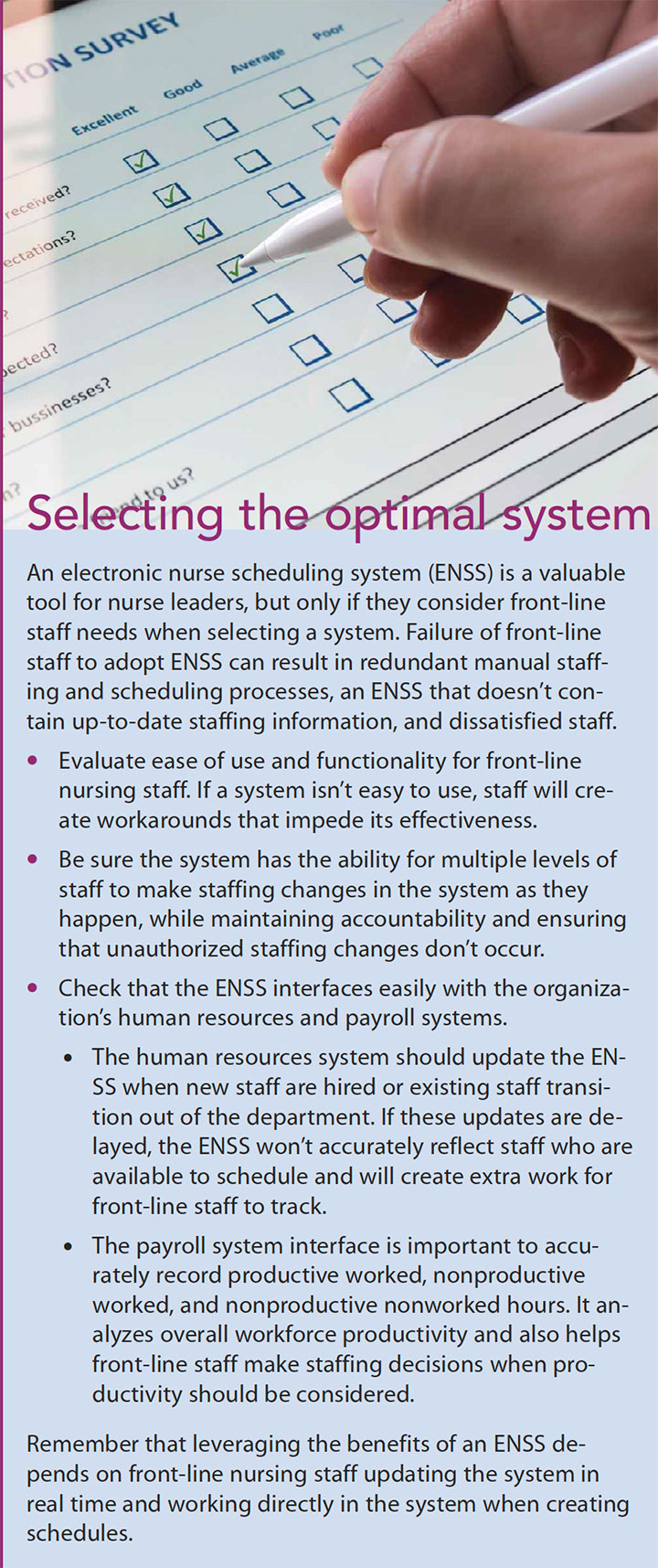
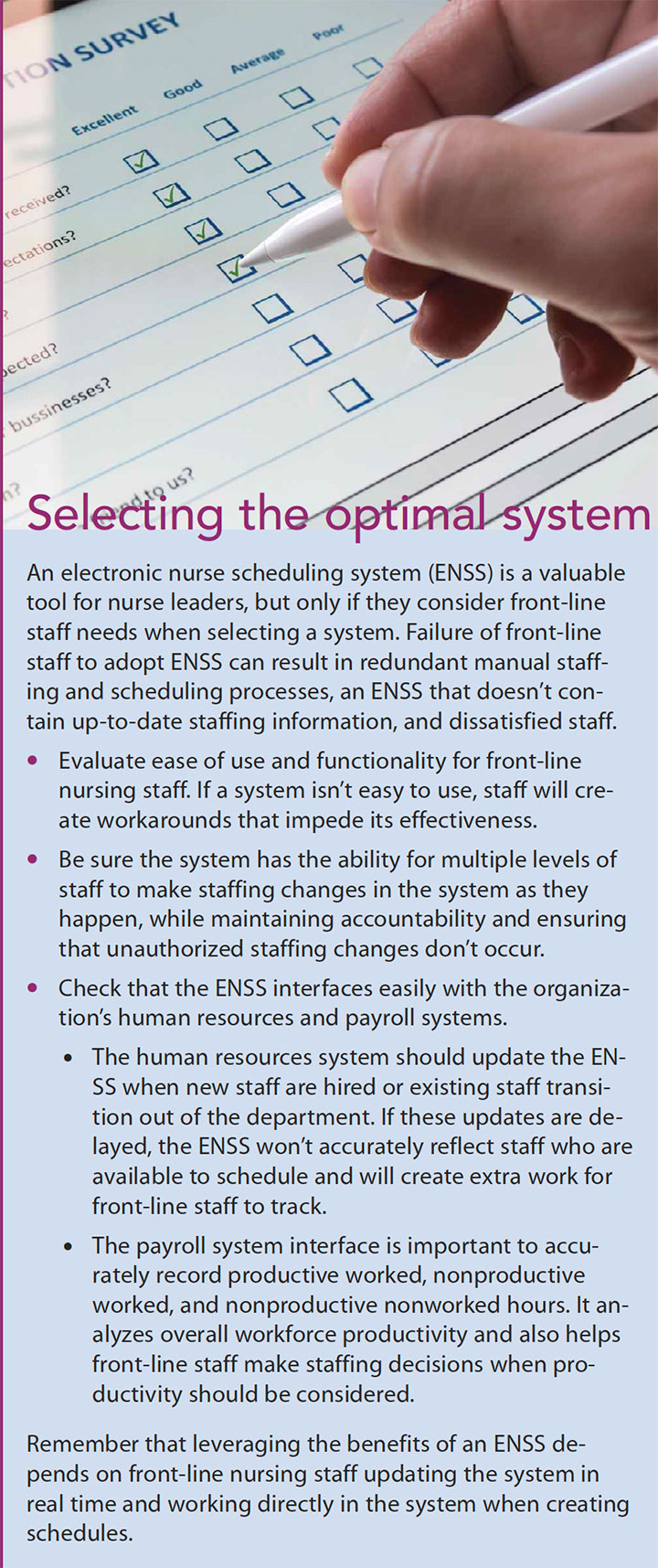
Investment in an ENSS can result in cost-effective delivery of high-quality patient care as well as staff satisfaction and retention. These systems support the decision making needed in complex delivery systems to ensure that resources are effectively allocated. They also pro- vide the platform to leverage staff expertise and input, and provide accountability in staffing and scheduling policies. An ENSS also tracks real-time financial performance, allowing leaders to proactively respond to potential challenges. Organizations must prioritize the need for investment in an ENSS to positively impact patient care, staff engagement, and operational efficiencies. And when choosing a system, leaders need to keep front-line staff interests top of mind (See Selecting the optimal system.)
Kathy Baker is the nursing director for emergency services and resource management at VCU Health in Richmond, Virginia and adjunct faculty at VCU School of Nursing. Kelton Rasmussen is interim business finance manager of patient care support administration at West Hospital VCU Health. The authors wish to acknowledge valuable insights for this article from Kevin Shimp, director of patient flow at VCU Health, who died earlier this year.
Selected references
American Nurses Association Nurse staffing. 2015. nursingworld.org/practice-policy/advocacy/state/nurse-staffing
Kane RL, Shamliyan T, Mueller C, Duval S, Wilt TJ. Nurse Staffing and Quality of Patient Care. Agency for Healthcare Research and Quality. March 2007. archive.ahrq.gov/downloads/pub/evidence/pdf/nursestaff/nursestaff.pdf
Koning C. Does self-scheduling increase nurse’s job satisfaction? An integrative literature review. Nurs Manag (Harrow). 2014;21(6):24-8.
O’Connor K, Dugan JL. Addressing floating and patient Safety. Nursing. 2017;47(2):57-8.













