For more than 20 years, the American Academy of Pediatrics (AAP) has encouraged everyone to place infants on their backs to sleep to help prevent sudden infant death syndrome (SIDS). The National Institute of Child Health and Human Development’s “Safe to Sleep®” campaign (launched as the “Back to Sleep” campaign in 1994) has had dramatic results: The number of infant deaths from SIDS and sudden unexpected infant death (SUID) has fallen a staggering 53% in 20 years.
In 2011, AAP expanded its 2005 recommendations to encompass the infant’s entire sleep environment. First Candle, a not-for-profit organization dedicated to safe pregnancies and infant survival, took this message to the public as “Safe Sleep Saves Lives.”
But despite decades of guidance from various organizations on what’s best for infants, as well as campaigns to promote safe sleep, as a pediatric nurse practitioner I find that safe sleep guidelines aren’t followed consistently. This article revisits the AAP recommendations on safe sleep and debunks myths, with a special focus on implications for practicing nurses.
Expanding the scope of recommendations
1. Here are the 18 recommendations issued by the AAP in 2011. Place infants to sleep on their back (supine). The slogan “Back to sleep” applies to all infants from 32 weeks postconceptual age in the neonatal intensive care unit to 12 months. When putting an infant down to sleep, place him or her on the back. Side sleeping isn’t recommended. However, if the infant independently rolls onto the abdomen, don’t roll him or her onto the back again; instead, allow the infant to stay in that position.
2. Use a firm sleep surface to decrease the risks of SIDS and suffocation. Use a crib, bassinette, or portable sleep environment that meets the safety standards of the U.S. Consumer Product Safety Commission and ASTM International (an organization that develops and delivers voluntary consensus standards). Make sure fitted sheets fit snugly on the mattress and the mattress fits snugly in the crib. Don’t let an infant sleep in a car seat or a swing.
3. Caution parents not to share a bed with their infant while sleeping, but encourage them to share a room with the infant. Bed sharing isn’t recommended with siblings, either (even with the infant’s twin). If a breastfeeding mother chooses to bring her infant to bed for feeding, she should return the infant to the crib (or bassinette or portable crib) once feeding is complete, before she goes to sleep. Any other person in the bed with the infant increases the SIDS risk. On the other hand, studies show SIDS risk decreases by nearly half when the infant shares a room (not a bed) with parents.
4. Keep soft objects and loose items out of the crib. These include bumper pads, wedges, sleep positioners, blankets, and pillows. Even a sleep positioner designed to reduce SIDS is unsafe. Avoid putting anything in the crib except a mattress, fitted sheet, and the infant. To provide warmth, blanket sleepers and sleep sacks are permitted.
5. Give the infant a pacifier at nap time and bedtime. Studies show this provides a protective effect. For breastfeeding infants, delay pacifier initiation until breastfeeding is well-established (around age 3 to 4 weeks).
6. Avoid overheating the infant. I usually advise parents to dress the infant in one layer more than what the parent is comfortable wearing. For example, a parent who dresses in shorts and a top should dress the infant in a “onesie” and add a knit or cotton sleep sack.
7. Teach women that breastfeeding helps reduce SIDS risk.
8. Encourage supervised “tummy time” while the infant is awake and alert, to promote optimal growth and development. Recommended duration and frequency haven’t been established. However, in my practice environment, the standard of care is to give the infant tummy time (when supervised and awake) with every diaper change for 5 to 10 minutes during the day. Tummy time promotes motor development and helps prevent positional plagiocephaly (head flattening).
9. Don’t use sleep positioners, wedges, special mattresses or sleep surfaces, or other commercial devices marketed to decrease SIDS risk. No evidence suggests these products offer protection, reduce suffocation risk, or are safe.
10. Encourage pregnant patients to get regular prenatal care to decrease SIDS and SUID risk.
11. Instruct women to avoid smoke exposure during pregnancy and after
delivery.
12. Caution women to avoid alcohol and illicit drug use during pregnancy and after delivery.
13. Advise parents not to use home cardiorespiratory monitors. These monitors haven’t been found effective in reducing SIDS risk. If parents ask your advice on buying an apnea monitor, inform them that although these monitors have value for some infants, no evidence supports the claim that they decrease SIDS incidence.
14. Urge parents to immunize the infant according to AAP recommendations and to take him or her for regular well-child checks.
15. Healthcare professionals, parents, and childcare providers should follow SIDS risk-reduction recommendations from the time of the infant’s birth.
16. Media and product manufacturers should follow safe sleep guidelines in their messaging and marketing materials. All media outlets and manufacturers should promote a safe infant sleep environment. Through a cooperative effort, safe sleep for infants can be modeled not just in the hospital and healthcare environment but also in print, television, and media messages.
17. The national campaign to reduce SIDS risk should be expanded to focus on the infant’s entire sleep environment—not just on sleep position. Family physicians and other primary care clinicians are encouraged to participate.
18. Ongoing SIDS research and surveillance are needed.
Implications for nurses
Safe infant sleep is a national priority. Healthy People 2020, a national health promotion and disease-prevention initiative, addresses safe infant sleep as a component of reducing SIDS and SUID incidence.
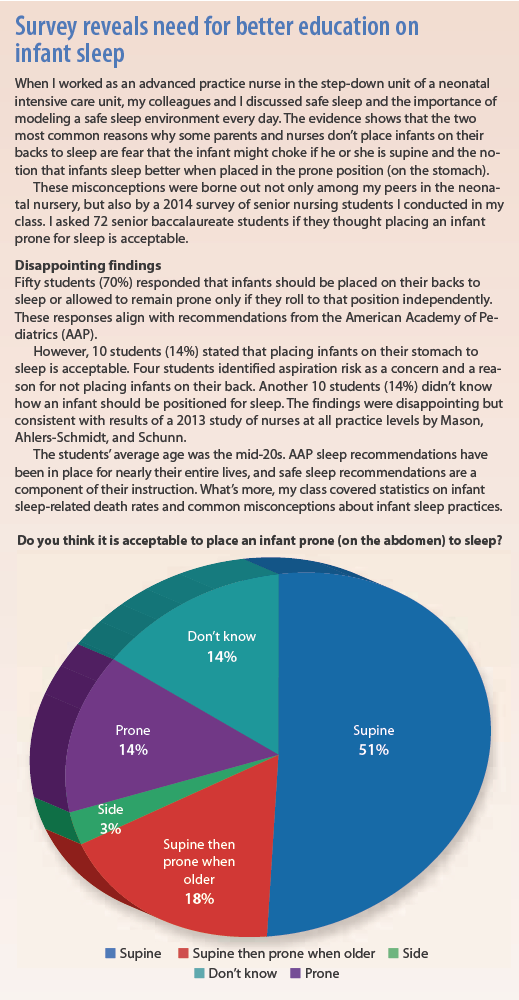
All healthcare professionals—especially those who provide direct patient care—must promote a safe infant sleep environment. We need to model safe, effective infant care; educate parents and caregivers; and promote components of a safe sleep environment. As nurses, we also need to educate each other. (See Survey reveals need for better education on infant sleep.)
What’s more, we need to provide consistent modeling and messages across all healthcare professions. Inconsistent caregiver modeling and messages causes confusion for parents, new nurses, and nursing students. As members of the most trusted profession, nurses are sought out by our communities for advice on health-related topics. We have a responsibility to give them evidence-based, consistent information. (See Using consistent, accurate messaging.)
Finally, nurses should contribute to standardized protocols and surveillance of SIDS and SUID and advocate for adequate funding of these efforts. Some researchers consider SIDS a completely preventable phenomenon. The urgency for action can’t be overstated.
Angela Lane is an assistant professor of nursing at Belmont University in Nashville, Tennessee. She worked as a pediatric nurse practitioner in Nashville for 8 years before transitioning to nursing faculty member.
Selected references
Hitchcock S. Endorsing safe infant sleep: a call to action. Nurs Womens Health. 2012;
16(5):386-96.
Mason B, Ahlers-Schmidt CR, Schunn C. Improving safe sleep environments for well newborns in the hospital setting. Clin Pediatr (Phila). 2013;52(10):969-75.
Murphy SL, Xu JQ, Kochanek KD. Deaths: Final data for 2010. Natl Vital Stat Rep. 2013;61(4):1-117.
National Institute of Child Health and Human Development. Safe to Sleep® Public Education Campaign. Last reviewed and updated January 2, 2015. nichd.nih.gov/sts/Pages/
default.aspx
Schnitzer PG, Covington TM, Dykstra HK. Sudden unexpected infant deaths: sleep environment and circumstances. Am J Public Health. 2012;102(6):1204-12.
Task Force on Sudden Infant Death Syndrome, Moon RY. SIDS and other sleep-related infant deaths: expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128(5):1030-9.



















1 Comment.
Thank you for providing concise safe sleep information. Under #1, the article includes the AAP recommendation for supine positioning, but not the AAP recommendations to rotate baby’s head and rotate baby’s position in the crib. Supine positioning is well known, not always head positioning, and parents need teaching on how to rotate the head to avoid or improve plagiocephaly, as well as tummy time mentioned in the article. In “Maternal Report of Advice Received for Infant Care” Staci Eisenberg et al conducted a 2015 nationally representative survey that quantifies advice received by 1,031 new mothers from 4 sources (doctors, nurses, family, media) on 5 infant care practices (breastfeeding, sleep position, sleep location, immunization, pacifier use). Breaking out sleep position, doctors and nurses provide advice consistent with recommendations just over 50% of the time. Advice is a modifiable factor that may influence a mother’s choice about infant care practices. As Dr. Lane suggests, standardized protocols will help to provide a consistent message. By educating parents and caregivers in the prenatal, hospital and clinic settings, nurses can create a culture of safe sleep practices.