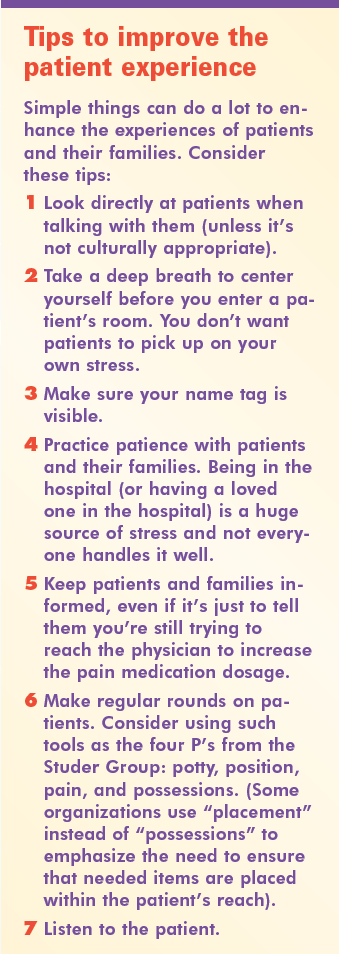
Promoting health and easing suffering—these goals lie at the heart of the essence of nursing. Given the many demands of nursing—call lights, phone calls, alarms, questions, and more—we can easily lose sight of that essence. To help remind us of the heartwarming, touching, and humorous aspects of being a nurse, we asked readers to send us their stories. (For ways to infuse the essence of nursing into your patients’ experiences, see Tips to improve the patient experience.)
Being a patient
Here are readers’ insights into being a patient.
The value of listening
Throughout my childhood, I spent a lot of time in and out of hospitals. During one stay, I met a nurse I’ll never forget. She came into my room and introduced herself. Although she was pleasant, I was a teenager and in a “mood.” I just wanted her to check my vitals, give me my medication, and leave me alone. She must have understood how I was feeling because after her introduction, she gave me medication and left the room.
Later that evening, she came back in. “How are you feeling?” she asked. “Fine,” I replied. She checked my vitals again and then sat down on the bed. “So, what are you working on?” she asked. This simple question sparked a long conversation about college and my dreams and ambitions, which seemed to last forever.
What made this moment so memorable? She listened. She asked questions that weren’t health related. She asked about me as a person and my homework. She cared about me as a person outside the hospital, beyond the “patient me.” She truly cared and was interested in me. It was enlightening, thoughtful and encouraging.
Carolyn Weese
Insights from the other side of the bed
Having practiced nursing for nearly 40 years, I know how to approach many healthcare situations. However, I found I wasn’t prepared to be a receiver of care. A few years ago, a diagnosis of breast cancer took me by surprise, throwing me into a whirlwind of information gathering and decision making. Although all aspects of my treatment (surgery, radiation, and chemo) were delivered in outpatient settings, I related the experiences to inpatient care. Here are some of the lessons I learned:
- As a patient, I had to be my own advocate. Don’t get me wrong: I had excellent healthcare providers. But none of them were mind readers. I was the only one who knew what I was experiencing, and I had to be very clear about what I needed to get through the process.
- For a healthcare provider to deliver appropriate care, he or she must demonstrate competence and compassion in equal measure. Doing the right things in the correct way with kindness and understanding is what the patient needs and deserves.
- Hope and encouragement, as well as doses of laughter, are important parts of every patient’s plan of care.
Carol Hatler, PhD, RN
Director, Nursing Research
St. Joseph’s Hospital & Medical Center, Phoenix, AZ
The little things
After several experiences of being on the other side of nursing care, I realized I prefer to be on the caring side. Nurses can be in control of the caring. A patient is at the mercy of caregivers.
I always wondered how patients can be so accepting of our care. When you’re sick, you don’t have the physical or emotional energy to even have a voice. Yet you search for the human side in your nurses. When you feel better, you want to show your appreciation. You remember even the little things, such as a housekeeper making sure you had water.
Loraine Strombeck, BS, RN
Easing the fear
As an RN going in to have a carotid endarterectomy, I knew too much for my own good. God must have put this certified registered nurse anesthetist on my case. He knew how terrified I was, and once he had his paperwork done and was waiting on me to go back, he pulled a chair up and talked to me. He showed me that I meant something to him, even though he’d never met me before, because I was human.
Nancy Creech, RN, MSN
Nurse Recruiter
Being a patient’s family member
These anecdotes recount what it was like for nurses whose loved ones were in the hospital.
Germs on the cell phone
Please wash your hands and always change your gloves! My husband, a microbiologist with more than 25 years’ experience, recently was admitted to his hospital of employment—an acute-care teaching hospital—for a sudden, life-threatening respiratory illness. As an experienced nurse (30+ years as an RN, 16 years as an APRN), I felt I needed to be with him 24/7.
Because of his “unknown infection,” he was prescribed a cocktail of highly vein-toxic antibiotics. The RN assigned to his care came in to establish a new I.V. site. During the procedure, she received a phone call on her hospital-assigned cell phone. She promptly answered the phone, responded to the call, and then returned to the procedure. My husband quickly stopped the procedure and stated, “Please change your gloves! Do you know how many germs are on your cell phone? Cellphones carry ten times more bacteria than most toilet seats.”
Antoinette Towle, EdD, APRN
Unforgettable nurses
I am an RN, but I was his wife, the mother of his child, and the one left with a hole in my heart that I thought would never close. He was my world and he was dying. I was helpless, but not hopeless. I’ll never forget his nurses—whether I saw them face-to-face or just knew they’d provided care for my husband. And I’ll never forget the support they gave to both him and me.
Nancy Creech, RN, MSN
Nurse Recruiter
In good hands
My grandson was only 10 months old when he had open-heart surgery for a major defect. While he was there, I discovered the true meaning of a Magnet®-recognized hospital.
In the pediatric open-heart ICU, all the nurses were pediatric CCRNs. Thank God! I knew he was in good hands. Now, at age 3½, he’s just fine.
Nancy Creech, RN, MSN
Nurse Recruiter
WTVAHCS
Humorous moments
These stories reflect the lighter side of nursing.
Blind date
For many years, I worked on an electrophysiology unit (cardiology stepdown), where many of the patients had life-threatening arrhythmias and required a calm, nonthreatening environment. I encouraged one of my frequently admitted patients to talk about his concerns and fears. This led to a discussion of what it was like to stay in the hospital for extended periods and be exposed to many different nurses and personalities. He told me, “It’s like having three blind dates a day. How stressful would that be?”
Peggy Newman RN,
MSN, PCCN
The art of pickling dentures
The transition unit was short staffed on the 3 pm-11 pm shift, so I volunteered to work. As I assisted a patient with his nighttime routine—cleaning his dentures—he placed his dentures in a small jelly jar with a denture cleanser tablet and water. He shook the jar and watched the tablet fizz, explaining, “I’m pickling my dentures!” We both laughed.
Julie Thibeau,
MSN, RN, CNOR
The incident of the bloody, naked man
The tall, kind gentleman was a blessedly normal patient who’d had a minor procedure, just staying overnight for observation. I passed meds and made sure he was set and safe for the night, then moved on to the rest of my wild bunch. I was lucky to be working with a fantastic nurse and an aide who was finishing nursing school and repeatedly tried to enlighten us on how to do our jobs properly.
In the middle of the night, this aide got up to find out what the noise in the hall was, and came running back to the desk, dead white. Upon inspection, I found my tall, kind gentleman naked and covered in blood, walking up the corridor. Rushing him back to his room, we found blood splattered everywhere. This easy, alert, and oriented patient had pulled out the I.V. line in his neck while sleeping in a chair in his room. He then walked across the room, went to the bathroom, and finally up the hall to us.
As the other nurse ran for bandages, I got him to his room while the aide stood motionless, in shock. Needless to say, he survived. We all did. When I took care of him the next night, he was so embarrassed. All he could say was he hoped never to see me again, knowing what I’d seen.
Stephenie Snodgrass,
MSN, RN-BC
An unexpected encounter
Spending so much time in the hospital growing up, I came across a lot of people. My doctors remained consistent, but I met a lot of different nurses, physical therapists, aides, and others. Of course, they’d encountered a lot of patients over the years. So it came as a surprise to me when I arrived at the hospital in the summer of 2001 for a normal procedure, and a bubbly nurse with brown curly hair came in the room and exclaimed, “I can’t believe you’re here.”
She went on to tell my parents and me how she normally works in the ER and was on duty when I was 3 months old and stopped breathing. She said even after she left the ER, she continued to think of me. She thought for sure I wasn’t going to make it and that if I did survive, I wouldn’t be a healthy, normal child. She was so surprised by how I had turned out. And I was surprised she remembered me 12 years later!
Carolyn Weese
Saved by an ED nurse
As nurses, we know that when we’re sick, we have an intrinsic desire to keep working. One mid-morning, I was working at a wound center when I started feeling ill with abdominal pain and chills. But the schedule was full and I felt the duty of patient care. As the hours ticked by, I started to feel worse, with nausea and confusion. The nurse I was working with called my husband to take me to the emergency department.
The emergency nurse greeted me with a smile, then began collecting lab samples and specimens and started I.V. normal saline solution. She saved my life by performing an expert emergent assessment and gathering a stool specimen immediately. Within 1 hour, I was diagnosed with nosocomial Clostridium difficile infection. The nurse administered I.V. metronidazole.
I was admitted to the hospital for 1 week, but didn’t need surgery. I’m so thankful to the emergency nurse who saved my life!
Helene Vossos, DNP, RN, ANP-BC, PMHNP-BC
Assistant Professor of Nursing
University of Michigan-Flint
Department of Nursing
Missed opportunity
Patient education and early warning signs are taught and reinforced to all nurses. Laparoscopic chlolecystectomy is a routine operation in any multispecialty hospital. When I was admitted for a relatively emergent “lap chole” in my own hospital, I was apprehensive. But the operation was uneventful, performed by a surgeon I’ve known for years and an anesthetist friend. I was transferred back to my room and my nurses were very attentive to my small needs.
Being on the heavier side, I was aware of the need for breathing exercises to prevent hypostatic pneumonia. But given my postsurgical pain and I.V. fluids, I needed someone to remind me of my breathing exercises. On day 3, I found my pulse rate creeping up and started to feel mild right-sided lower chest pain, exaggerated on deep breathing.
I called my intensivist friend and asked him to auscultate my chest. He found I had impending hypostatic pneumonia—caught in the nick of time. I took this opportunity to help my nurses on the unit reflect on how they’d missed my slightly increasing pulse rate and respiratory rate and had failed to remind me to do deep breathing and spirometry exercises. A classical example of the gap between theory and practice.
Thankam Gomez



















1 Comment.
The sacred encounter with a house supervisor..
I am a med surge nurse worked in the same hospital for 33 years. At the time I was a nurse manager of the med surge/Gyn unit. My husband was 50 years old and suffered a traumatic brain injury after surgery for a dissecting aortic aneurysm (Type 1). It was a rough day post operatively, and I had not left my husbands bedside for 3 days. There was a sleeping chair in the room for me.
It was about 3 in the morning and I could not sleep, I was so worried about my husband. I started cleaning out my purse. The house supervisor came into the room and wondered what I was doing. When I told her I was cleaning out my purse, she sat beside me and began to help me. We sat there and just talked. She provided me with comfort and compassion, sitting next to me and helping me clean out my purse.
Cherri Salesky