How clinical faculty and practicing clinicians can collaborate to help students learn professionalism.
Takeaways:
- Professionalism creates the foundation for civil and healthy work environments.
- According to the American Nurses Association, a healthy work environment is one that is safe, empowering, and satisfying.
- Using the Form, Storm, Norm, Perform, and Adjourn method of team formation, teams of clinical faculty and practicing clinicians can collaborate to help students learn professionalism.
Professionalism (the integration of professional values in the workplace via words and conduct), which is embedded in the Code of Ethics for Nurses With Interpretive Statements and nurse practice acts, creates the foundation for civil and healthy work environments that are safe, empowering, and satisfying. Healthy work environments, which are cultivated through open and purposeful communication among interprofessional groups, support optimal care delivery and ensure positive patient outcomes.
Essential competencies—such as effective, efficient communication and collaboration among interprofessional healthcare teams—have been cited by the Institute of Medicine and others as lacking in many new graduate nurses. Preparing new nurses for practice requires dedicated and coordinated responses from academic and practice organizations. According to Clark, professional skills are similar to clinical skills; both can be learned and improved upon over time using strategies and appropriate role modeling. (See Model behaviors.)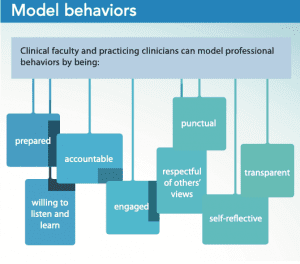
By understanding shared responsibilities and building effective teams, faculty, clinicians, and students can collaborate to instill professionalism and build healthy work environments.
Shared responsibility
Rather than feeling mentored and nurtured, many students report feeling unwelcome in the clinical environment, which leads to isolation, emotional distress, depression, and fear about their career future. Unhealthy work environments pose a threat to nursing student learning, new graduate transition, job satisfaction, employee retention, professional development, and patient safety. We stand little chance of breaking the chain of workplace incivility if the next generation of nurses believes this type of behavior is acceptable. Reasons behind our current dilemma are multifaceted, and everyone—clinical faculty, nurse managers, staff nurses, and students—plays a role.
Clinical faculty
Clinical faculty, even when they’re on the unit, may not always be “present” for students because students may feel their instructors are unapproachable. This frequently is a result of perceived incivility. For example, some faculty may reprimand students in the presence of others, leaving students feeling insecure and belittled. In addition, faculty may be responsible for eight to 10 students at a time, which can be overwhelming, especially during medication administration, creating stress that can carry over to how faculty respond to students.
Nurse managers
Different nursing programs have varying numbers of clinical hours and objectives. With several clinical groups assigned to one unit, nurse managers may struggle to keep track of them, creating a hurdle when managers need to speak to instructors about student issues. In addition, some nurse managers may not trust faculty, may believe students are disruptive to unit workflow, and may not see themselves as having a stake in educating future nurses. And if nurse managers speak inappropriately to or discipline staff or students, they foster the impression that incivility is allowed.
Staff nurses
Staff nurses may not see themselves as stakeholders in educating future nurses. Staff may believe that teaching professionalism is the clinical instructor’s job, not theirs, making them less likely to participate in the process.
Students
Students may have an idealized view of nursing and struggle when reality doesn’t fit that view, which can be a barrier to open communication.
Building partnerships
When clinical faculty and clinicians use the form, storm, norm, perform, adjourn method of team formation, they can collaborate to create a partnership built on professional standards and a shared vision, while teaching students professionalism.
Forming
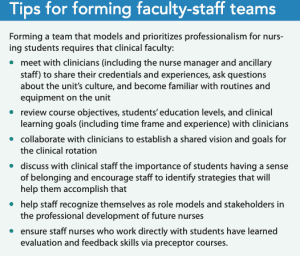
Initially, clinical staff may be unclear about their roles and responsibilities with regard to nursing students or view their work with them as an unpaid burden. At this first stage of team development, clinical faculty and practicing clinicians must be clear about tasks and debunk the myths (for example, about how nurses only follow physicians’ orders, that learning ends when you get your degree, and that male nurses are needed mainly for the heavy work) that contribute to unprofessionalism. (See Tips for forming faculty-staff teams.)
Storming
At this stage, conflict may exist between faculty and staff team members. Some staff may even rebel against assigned tasks because they don’t trust the faculty member’s clinical skills and they aren’t certain of a student’s ability to safely care for patients. Open communication is essential to create an atmosphere for sharing ideas, building mutual respect, and solving problems. Because approximately 80% of communication is nonverbal, everyone must be coached to be mindful not only of verbal communication, but also of body language (for example, facial expressions and posture) when collaborating with each other and caring for patients.
Everyone also should learn to use conflict constructively; it should never become personal. Instead, for example, if conflict arises about how to approach a learning experience, staff, students, and the clinical instructor should brainstorm to establish alternative, mutually agreed upon plans. TeamSTEPPS®, a tool created by the Department of Defense’s Patient Safety Program in collaboration with the Agency for Healthcare Research and Quality, can help identify possible reasons for conflict and support the team through this stage. (See The perfect storm.)
Everyone—clinical faculty, students, staff nurses, and nurse managers—has a role to play in establishing a team that prioritizes and models professionalism and collaboration to promote effective communication and problem-solving.
Tips for clinical faculty
- Be approachable.
- Seek input from the nurse manager and nursing staff about student nurse pairing and patient assignments.
- Encourage conversations where clinical staff feel free to give honest feedback about clinical and communication skills and developing effective collegial relationships.
- Acknowledge the prevalence and effects of incivility and implement policies and strategies to reduce incivility toward nursing students.
- Perform a daily formative evaluation of the clinical environment and a summative evaluation at the end of the clinical rotation.
- Check in with nurses and students; ask, “How’s it going? How can I help?”
Tips for students
- Be engaged, assertive, and respectful.
- Prepare an elevator speech (short, succinct, effective, and delivered enthusiastically) so you can introduce yourself to busy unit nurses and communicate intentions, passions, and learning goals.
- Take responsibility for meeting clinical objectives.
- Demonstrate an inquiring mind by asking questions and seeking clarification.
- Contribute meaningfully to the unit’s routine by offering assistance to both staff and patients.
Tips for staff nurses
- Encourage students.
- Share your expertise and experiences.
- Speak up. If you’re overwhelmed with patient care, let the charge nurse, nurse manager, or clinical instructor know. They’re there to support you.
- Be honest, but kind, when providing feedback. Remember, you’re preparing your future colleagues for professional practice.
Tips for nurse managers
- Be present and available. Be visible on the unit; establish an open-door policy; allot time to spend with staff, students, and faculty; listen and speak with intention; and be engaged.
- Listen and maintain open lines of communication with the clinical instructor, staff, and students.
- Share past student clinical experiences with staff and students.
- Clearly define roles and boundaries that adhere to scope of practice and organizational policies early in the rotation to ensure expectations are understood.
- Pause before you speak, so information is delivered calmly and thoughtfully.
- Model professional behavior.
- Remember the Platinum Rule: Treat others the way they would like to be treated.
Norming
Generally accepted procedures and communication patterns are established during this stage to promote bonding and group identity. The team begins to identify each member’s strengths and build on them together, and everyone understands their roles and begins working together for the greater good—investing in nursing’s future and ultimately improving patient outcomes. As committed partners, the team is relentless in pursuing and fostering true collaboration.
Performing
The team begins to focus all of its attention on achieving shared goals. Everyone is close and supportive, open and trusting, resourceful and effective. Leaders meaningfully recognize and celebrate the accomplishments of the whole team, which fully embraces the imperative of a healthy work environment—authentically living it and engaging others in its achievement.
Adjourning
At the end of the student’s clinical experience, all team members should have the opportunity to reflect on the experience, objectively critique successes, evaluate areas for improvement, and identify best practices for the future.
Benefits of teaching professionalism
Incorporating strategies to develop professionalism into every aspect of clinical education has far-reaching, positive implications. Not only can healthcare teams pre-empt problems before they arise, but also teamwork prepares students for a future in which they model professionalism, work to create and sustain healthy work environments, and learn the skills to diffuse conflict. Teaching professional behavior also prepares students for practice by helping them realize and accept the full breadth of nursing, including the values, morals, and attitudes embraced by the profession. Socializing future nurses into the profession, which is the responsibility of clinical faculty and practicing nurses, benefits nursing and patient care in a variety of ways. Students will:
- assimilate knowledge, use skills learned in clinical, and carry both into the workplace
- receive mentoring, observe role models, and engage in meaningful learning opportunities
- develop professional skill sets that decrease incivility and increase healthy work environments
- continue to develop professionally throughout their careers—a key factor in obtaining positive patient outcomes.
Potential challenges
Some clinical faculty or staff may be unable or unwilling to adhere to the team-building process because of staff shortages, increased patient acuity, limited knowledge of learning outcomes, or an unwillingness to participate. However, without consistency and collaboration between clinical faculty and staff, the team-building process will lack cohesiveness and continuity. The National League for Nursing proposed promoting academic partnerships to enhance collaboration between faculty and clinical staff, ensure all team members feel valued, and establish clear roles. Clear communication, mutual respect, and faculty willingness to support students and staff facilitate a cohesive work environment.
Preparing tomorrow’s colleagues
Creating healthy clinical work environments leads to more engaged nurses, decreased burnout, reduced turnover, and better patient care. In addition, staff nurses will recognize themselves as mentors and stakeholders in preparing future nurses for practice. As the saying goes, today’s students are tomorrow’s colleagues.
Kimberly Dimino is an assistant professor in the department of nursing at William Paterson University in Wayne, New Jersey, and a nurse scientist at Hackensack Meridian Health in Hackensack, New Jersey. Joset Brown is an assistant professor in the department of nursing at William Paterson University. Bea Fernandes is a nurse manager at St. Joseph’s Children’s Hospital in Paterson, New Jersey.
References
Agency for Healthcare Research and Quality. About TeamSTEPPS. June 2019. ahrq.gov/teamstepps/about-teamstepps/index.html
American Association of Critical-Care Nurses. AACN standards for establishing and sustaining healthy work environments: A journey to excellence. Am J Crit Care. 2005;14(3):187-97.
American Nurses Association. Code of Ethics for Nurses With Interpretive Statements. 2015. nursingworld.org/practice-policy/nursing-excellence/ethics/code-of-ethics-for-nurses/coe-view-only
Babiker A, El Husseini M, Al Nemri A, et al. Health care professional development: Working as a team to improve patient care. Sudan J Paediatr. 2014;14(2):9-16.
Benner P, Sutphen M, Leonard V, Day L. Educating Nurses: A Call for Radical Transformation. San Francisco, CA: Jossey-Bass; 2010.
Blake N, Collins M. Importance of healthy work environment education in nursing schools. AACN Adv Crit Care. 2017;28(3):289-90.
Clark CM. Fostering a culture of civility and respect in nursing. J Nurs Regul. 2019;10(1):44-52.
Dimino K, Louie K, Banks J, Mahon E. Exploring the impact of a dedicated education unit on new graduate nurses’ transition to practice. J Nurses Prof Dev. 2020;36(3):121-28.
Edgecombe K, Wotton K, Gonda J, Mason P. Dedicated education units: 1. A new concept for clinical teaching and learning. Contemp Nurse. 1999;8(4):166-71.
Hofler L, Thomas K. Transition of new graduate nurses to the workforce: Challenges and solutions in the changing health care environment. N C Med J. 2016;77(2):133-6. ncmedicaljournal.com/content/77/2/133.full
Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. Washington, DC: National Academies Press; 2011.
Kavanagh JM, Szweda C. A crisis in competency: The strategic and ethical imperative to assessing new graduate nurses’ clinical reasoning. Nurs Educ Perspect. 2017; 38(2):57-62.
Knight CC, Hamilton SH. Getting students to value leadership early in the nursing curriculum: Innovation makes it possible. Nurs Educ Perspect. 2019;40(4):254-6.
National League for Nursing. Interprofessional Collaboration in Education and Practice. December 2015. nln.org/docs/default-source/default-document-library/ipe-ipp-vision.pdf?sfvrsn=14
Natvig D, Stark NL. A project team analysis using Tuckman’s model of small-group development. J Nurs Educ. 2016;55(12):675-81.
Oja KJ. Incivility and professional comportment in critical care nurses. AACN Adv Crit Care. 2017;28(4):345-50.
Pagana KD. Ride to the top with a good elevator speech. Am Nurse Today. 2013;(3). myamericannurse.com/ride-to-the-top-with-a-good-elevator-speech
Simpson KR. Incivility, bullying, and workplace violence: New recommendations for nurses and their employers from the American Nurses Association. MCN Am J Matern Child Nurs. 2016;41(1):68.
Segal J, Smith M, Robinson L, Boose G. Nonverbal communication. June 2019. helpguide.org/articles/relationships-communication/nonverbal-communication.htm
Tecza B, Boots BK, Mains BC, et al. Incivility toward nursing students in clinical rotations: Measuring the incidence and testing interventions. J Nurs Admin. 2018; 48(11):585-90.
Tuckman BW, Jensen MAC. Stages of small-group development revisited. Group & Organization Studies. 1977; 2(4):419-27.
Woolforde L. Beyond clinical skills: Advancing the healthy work environment. J Nurses Prof Dev. 2019;35(1):48-9.
World Health Organization. Being an Effective Team Player. who.int/patientsafety/education/curriculum/who_mc_topic-4.pdf
Zhu Z, Xing W, Lizarondo L, Guo M, Hu Y. Nursing students’ experiences with faculty incivility in the clinical education context: A qualitative systematic review and meta-synthesis. BMJ Open. 2019;9(2):e024383.