Teamwork ensures prompt and appropriate care.
- Cystic fibrosis, an autosomal recessive genetic disorder, involves loss of normal protein function, which leads to mucous obstruction in the lungs.
- Exacerbations of cystic fibrosis frequently require complex ventilator management.
- Early recognition of clinical deterioration and effective team communication aids prompt and appropriate treatment.
Amelia Fantano*, a 48-year-old woman with a history of cystic fibrosis (CF), is admitted to the surgical unit with a small bowel obstruction. At home, Ms. Fantano wears three liters of oxygen via nasal cannula, which she continues while hospitalized. Her obstruction is managed conservatively with nasogastric tube decompression and I.V. fluids.
Troy, Ms. Fantano’s nurse, notes bilateral rhonchi and a soft, non-tender, mildly distended abdomen during his initial assessment. As Troy helps the patient out of bed, she experiences a coughing episode that results in a decrease in SpO2 to 83%. Troy assists Ms. Fantano back to bed and places her in the high Fowler position. When he reassesses her lungs, he hears inspiratory and expiratory wheezes and notes that the patient is more tachypneic. The respiratory therapist provides a nebulizer treatment, and Troy confirms that the ordered mucolytic medication was given earlier that morning.
The changing face of cystic fibrosis
Despite these interventions, Ms. Fantano’s SpO2 doesn’t rise above 85%. Troy initiates a 100% non-rebreather mask, but the patient’s work of breathing remains high and she’s unable to speak in full sentences. Troy initiates a rapid response.
On the scene
When the team arrives, they note the patient’s labored breathing and the use of accessory muscles. Her vital signs are temperature 98.4° F, HR 120 bpm, RR 32 breaths per minute, BP 131/87 mmHg, and SpO2 88% on 100% non-rebreather mask. Her abdominal assessment is benign.
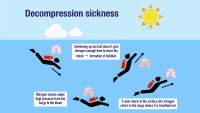
The provider orders an ABG to assess Ms. Fantano’s ventilation and oxygenation. Given the patient’s ongoing increased work of breathing and high oxygen requirement, the respiratory therapist recommends high-flow nasal cannula (HFNC) 100% 50 L to provide further respiratory support with increased flow rate and for patient comfort.
Troy prompts the provider to order I.V antibiotics and a chest x-ray. Despite all interventions, Ms. Fantano continues to deteriorate. The ABG reveals a low PaO2/FiO2 ratio and hypercarbia. Concerned about impending respiratory failure, the team recommends transfer to the MICU for advanced ventilatory support.
While waiting for the MICU bed, Troy places an additional peripheral I.V. in anticipation of intubation. The patient is transported to the MICU and safely intubated.
Debriefing
The team conducts an interprofessional safety debriefing. Because the patient experienced an acute desaturation, no concern exists about missing early clinical deterioration. The team agrees that HFNC was an appropriate interim solution given the patient’s discomfort with BiPap, and they agree that transferring the patient to the MICU was the best option. The nurses note that they have little experience with patients with CF. The clinical nurse specialist creates a tip sheet for the staff in anticipation of the patient returning to the unit.
Education
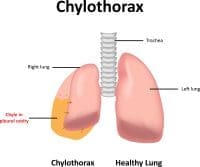
CF, an autosomal recessive genetic disorder, involves loss of normal protein function, which leads to mucous obstruction in the lungs. Many people with CF have chronic bacterial lung infections that result in a localized inflammatory response and recurrent mucous plugging. The disease can lead to structural lung damage and loss of lung function. CF also can cause pancreatic insufficiency and biliary cirrhosis, resulting in liver failure, which, according to Shteinberg and colleagues, remains the third leading cause of death for those with CF.
Long-term management of CF includes airway clearance techniques, mucolytic medications, airway surface hydration, and inhaled antibiotics in the setting of chronic pseudomonal lung infection. Exacerbations of CF occur and frequently require complex ventilator management.
*Names are fictitious.
Megan Holland is a nursing clinical coordinator at Penn Medicine in Philadelphia, Pennsylvania. Joanne Phillips is a nursing administrative coordinator at the Hospital of the University of Pennsylvania in Philadelphia.
American Nurse Journal. 2024; 19(11). Doi: 10.51256/ANJ112414
References
Ong T, Ramsey B.W. Cystic fibrosis: A review. JAMA. 2023;329(21):1859-71. doi:10.1001/jama.2023.8120
Shteinberg M, Haq IJ, Polineni D, Davies JC. Cystic fibrosis. Lancet. 2021;397(10290):2195-2211. doi:10.1016/s0140-6736(20)32542-3
Key words: interdisciplinary communication, collaboration, respiratory management