Nurses need to understand the nuances of this therapy.
Takeaways
- Nurses should know the risks, benefits, and controversy surrounding high-flow nasal cannulas in adults with COVID-19.
- Nurses should be able to implement, monitor, and evaluate patients receiving high-flow nasal cannula therapy.
Editor’s note: This article is an early release web exclusive article for the October 2020 issue of the American Nurse Journal.
Novel and unconventional strategies continue to emerge in response to the SARS-CoV-2 virus (COVID-19). One recent innovative response is high-flow nasal cannula (HFNC) use for adults experiencing the respiratory effects of COVID-19. HFNC provides warmed, humidified oxygen at higher fractions of inspired oxygen (FiO2) levels and flow rates than conventional oxygen therapy, potentially reducing the number of patients requiring intubation and mechanical ventilation. Increased HFNC use stems from an attempt to mitigate the virus’s devastating pulmonary effects, including alveolar inflammation that leads to scarring and respiratory compromise, which persist after the virus has been treated.
However, HFNC is controversial because of limited and inconsistent research and the risk for aerosolization of virus particles. This article discusses the delivery of HFNC, its benefits and risks, and nursing considerations.
HFNC delivery
Recommendations for traditional nasal cannulas were initially limited to low-flow oxygen rates up to 6 L/min to reduce patient discomfort and mucosal tissue drying. In the early 2000s, clinical studies emerged on the use of HFNCs (up to 40 L/min) that could achieve FiO2 levels comparable to or higher than non-rebreather masks. By using warmed and humidified oxygen, HFNC reduces mucosal drying. In perinatal care, healthcare providers have used HFNC for several decades to treat premature neonates with respiratory distress syndrome. Now it’s being used with adults for COVID-19–related acute respiratory failure and hypoxemia when noninvasive ventilation is preferred.
Usually, HFNC is offered with heated, humidified air; although nonheated options are available. It can be titrated at different FiO2 levels based on manufacturer recommendations. Oxygen is delivered through a wide-bore, nasal cannula with flow rates typically at 20 to 35 L/minute (flow rates can go as high as 60 L/minute) and FiO2 ranging from 21% to 100%, depending on the patient’s clinical response. Patients can be weaned down to a conventional low-flow nasal cannula when appropriate (usually 1 to 6 L/minute or per facility protocol). HFNC is most appropriately used in monitored units—such as ICUs, step down units, or emergency departments—with pulse oximetry alarms.
Benefits
With warmed humidification to hydrate airways, HFNC provides many respiratory benefits in addition to improved oxygenation. It decreases cardiac and breathing workload, which directly reduces carbon dioxide production, and it reduces dead space in the lungs by increasing surface area available for gas diffusion and providing positive airway pressure (continuous positive airway pressure [CPAP] effect). In addition, HFNC helps reduce the body’s energy workload by reducing inspiratory effort, improving lung compliance, and by increasing mucus and ciliary function, resulting in decreased caloric expenditure. The low-level positive pressure generated by HFNC increases lung volume and improves gas exchange when oxygen flow is maintained at the highest level tolerated by the patient. Avoiding mechanical ventilation and intubation may reduce long-term complications such as infections, tracheostomies, and scarring.
Clinical studies show a greater patient acceptance and comfort level for HFNC when compared with standard masks or non-rebreather masks. This may be attributed to being able to eat, drink, and speak more easily. HFNC also can reduce the claustrophobia some patients experience when wearing facemasks. (See HFNC vs. mechanical ventilation.)
High-flow nasal cannula (HFNC) offers some benefits over mechanical ventilation.
| HFNC | Mechanical ventilation |
| · Increased patient comfort | · Potential irritation to trachea
· Sedation needed |
| · Noninvasive
· Potential need for emergency intubation and mechanical ventilation if HFNC fails |
· Invasive
· Potential need for tracheostomy if unable to be removed from ventilator · Other long-term complications such as infection |
| · Patients can communicate, eat, and drink | · Patients sedated with communication deficits
· Need for alternative feeding routes · Potential for malnutrition |
| · Limited mobility possible | · Immobility complications (constipation, fall, debility, pressure injuries) due to bedrest |
Risks and controversies
HFNC is one of several modalities for noninvasive ventilation; the European Society of Intensive Care Medicine suggests HFNC as first-line therapy for patients with COVID-19. However, concern persists that HFNC high-flow rates may increase airborne transmission of the virus via aerosolization. This concern has led many healthcare facilities to create policies limiting bag-mask and CPAP and bilevel positive airway pressure device use in patients with suspected or confirmed COVID-19. Risk of healthcare worker infection from virus particles spreading in the environment is directly correlated with the flow rate of these devices.
To reduce this risk, patients on HFNC are placed in private, negative-pressure, airborne isolation rooms with anterooms. Staff use full personal protective equipment (PPE) for airborne precautions, including water-resistant gowns, N95 masks, face shields or goggles, and gloves. Many organizations that use HFNC require patients to wear a surgical mask when staff are in the room to reduce the risk of aerosolization, but this practice hasn’t been well-studied for safety. Surgical masks may reduce carbon dioxide clearance, so nurses and other healthcare workers should limit the time patients on HFNC wear surgical masks, watch for increased work of breathing during mask wearing, and titrate FiO2 as necessary. Although no absolute contraindications to HFNC exist, its use should be carefully considered in patients with an altered level of consciousness on the Glasgow Coma Scale, reduced upper airway reflexes, epistaxis, claustrophobia, risk for aspiration, or unstable hemodynamics.
The lack of research documenting improved clinical outcomes, such as reduced mortality and decreased need for mechanical ventilation, has led some healthcare providers to believe HFNC hasn’t met the threshold of doing more good than harm. In fact, current research indicates that HFNC doesn’t improve overall patient mortality, even though patients tolerated HFNC better than conventional oxygen therapy. Some healthcare providers believe this lack of research means the respiratory status of patients on HFNC will continue to decline, resulting in emergency intubation and mechanical ventilation. Rather than HFNC, some experts advocate early intubation for patients with deteriorating respiratory status who require more than 6 L/min of oxygen. This approach may be reasonable when ventilators aren’t in short supply. More research on the prevalence of HFNC failure is needed to draw definitive conclusions.
Nursing implications
To reduce healthcare worker exposure to the virus and promote optimal patient care, several actions must be considered. Nurses and hospital administration should work together to ensure sufficient staff to care for patients on HFNC and reduce exposure, and they should closely follow emerging evidence on virus transmission and safe care practices. (See HFNC overview.)
Understanding how high-flow nasal cannula (HFNC) works, the steps for providing treatment, and proper monitoring and management will help ensure good patient outcomes.
Mechanisms of action
HFNC:
- provides noninvasive oxygenation with precise and higher FiO2 levels that can be titrated based on patient needs
- uses warmed gas to minimize airway constriction; humidification keeps respiratory mucosa moist for comfort and respiratory secretion mobilization
- uses positive airway pressure to keep alveoli open, reduce dead space, and improve gas exchange
- washes out anatomical dead space and decreases carbon dioxide to improve ventilation
- decreases breathing workload and energy expenditure.
Set-up
Follow these steps for setting up HFNC:
- Collect proper equipment, including correct size of nasal prong and tubing length. You may have to choose between small or larger adult sizes depending on the manufacturer.
- Ensure humidification fluid is in place and heating circuit is functioning. A dust filter may be used over the room air intake port.
- Adjust the flow rate first, then titrate FiO2 to appropriate levels.
- Insert the cannula into the patient’s nostrils and secure it to the patient’s head with an elastic strap to prevent lateral air loss.
- Monitor the patient’s skin surrounding the nostrils under and around HFNC to identify potential skin breakdown or pressure injuries.
- Adjust the head strap to patient’s head, carefully avoiding the ears; don’t overtighten.
- Secure the head strap clip to the nasal cannula and clip HFNC tubing to the patient’s gown to relieve tension.
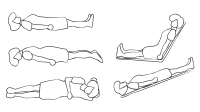
- Maintain the patient in semi-Fowler’s position and consider periodic prone positioning to promote lung expansion.
- Ensure suction equipment is present in the room.
- Monitor the patient for comfort and tolerance.
Nursing care
Your nursing care of patients on HFNC should include the following:
- Educate the patient about the need for frequent coughing and deep breathing exercises.
If you’re caring for patients with COVID-19 who are on HFNC, follow these steps to reduce viral particle spread:
- Don and doff all PPE in the correct order.
- Dispose of or clean PPE properly.
- Adhere to strict surface and equipment decontamination practices.
- Cluster care to limit patient contact and reduce exposure risk.
- Place a surgical mask over the patient’s HFNC device to reduce viral aerosolization when in the room.
- Avoid transporting patients out of their rooms.
- Ensure that patients are placed in a negative-pressure room to allow for ventilation with regular air exchanges.
Properly fitted cannula
A properly fitted cannula reduces the risk of facial pressure injuries and healthcare staff exposure to aerosolized virus particles. Completely insert the cannula into the patient’s nostrils and secure it with elastic straps to the patient’s head to prevent lateral air loss. Ensure the strap around the head isn’t over the patient’s ears and adjust it to fit the head without overtightening; the head strap clip should be securely attached to the nasal cannula.
The nasal prong diameter should be approximately half the size of the patient’s nostrils to reduce the risk of air leak and resulting loss of positive airway pressure and potential virus aerosolization. Having small adult/pediatric and adult size nasal cannulas readily available will help ensure proper fit. Maintain the patient in semi-Fowler’s position and use periodic prone positioning to aid lung expansion and redistribute pulmonary blood flow to increase perfusion. Ensure suction equipment is easily accessible, and teach patients coughing and deep breathing exercises to clear the lungs.
Patient monitoring and assessment
The greatest concern for patients on HFNC is the need for emergent intubation if treatment fails, so your early recognition of changes in the patient’s condition is essential. Track trends in vital signs and look for any increased work of breathing (elevated heart rate, elevated respiratory rate, blood pressure changes, and decreased oxygen saturation levels). Titrate oxygen flow rates according to the patient’s respiratory rate and work of breathing for a targeted oxygen saturation no higher than 96% or per facility protocol. Monitor the patient for potential respiratory compromise such as declining oxygen saturation (as measured by pulse oximetry), tachypnea, use of accessory muscles, intercostal recession, abdominal distension, secretions in the tubing, and changes in lung sounds. Measure arterial blood gases daily and watch for FiO2 titrations or changes in patient condition. Interpret and report results to the provider immediately.
The American Heart Association recommends that providers assess patients at 1 hour and 3 hours after HFNC initiation to determine response and whether intubation should be considered. Intubation shouldn’t be delayed if the patient isn’t improving.
Stay knowledgeable
A growing body of evidence supports the use of HFNC as an effective modality for early treatment of adults with hypoxemia and respiratory failure, including those with COVID-19. Front line nurses must be knowledgeable about the benefits and risks of this therapy and consult with the interprofessional team, including respiratory therapists and providers, as needed. As more research emerges and hospital policies evolve, nurses must stay knowledgeable about evidence-based practices and advocate for the best oxygen delivery methods.
Janet M. Reed is an associate lecturer in nursing at Kent State University at Stark in North Canton, Ohio. Tracy Dodson is a lecturer, clinical faculty, and course coordinator at the College of Nursing, Kent State University in Kent, Ohio. Richard E. Ferdig is summit professor of learning technologies in the Research Center for Educational Technology at Kent State University.
References
Alhazzani W, Møller MH, Arabi YM, et al. Surviving Sepsis Campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. 2020:1-34.
American Heart Association. Oxygenation and Ventilation of COVID-19 patients. 2020. cpr.heart.org/-/media/cpr-files/resources/covid-19-resources-for-cpr-training/oxygenation-and-ventilation-of-covid-19-patients/ovcovid_mod1_nppvhfnc_200401_ed.pdf?la=en&hash=8DA0793B37E4A28DE120BEB7003ACEC46CA28148
Davenport L. Noninvasive ventilatory support in COVID-19: Friend or foe? Medscape. 2020. medscape.com/viewarticle/928259#vp_2
Galiatsatos P. What coronavirus does to the lungs. John Hopkins Medicine. April 13, 2020 hopkinsmedicine.org/health/conditions-and-diseases/coronavirus/what-coronavirus-does-to-the-lungs
Gattinoni L, Chiumello D, Caironi P. et al. COVID-19 pneumonia: Different respiratory treatments for different phenotypes? Intensive Care Med. 2020;46(6):1099-1102.
Helviz Y, Einav S. A systematic review of the high-flow nasal cannula for adult patients. Crit Care. 2018;22(1):71.
Hernández G, Roca O, Colinas L. High-flow nasal cannula support therapy: New insights and improving performance. Crit Care. 2017;21(1):1-11.
Loh N, Tan Y, Taculod J, et al. The impact of high-flow nasal cannula (HFNC) on coughing distance: Implications on its use during the novel coronavirus disease outbreak. Can J Anaesth. 2020;67(7):893-4.
Mauri T, Turrini C, Eronia N, et al. Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med. 2017;195(9):1207-15.
Rali AS, Nunna KR, Howard C, Herlihy JP, Guntupalli KK. High-flow nasal cannula oxygenation revisited in COVID-19. Card Fail Rev. 2020;6:e08.
Tiglis M, Neagu TP, Diaconu C, et al. The importance of high flow nasal cannula (HFNC) oxygen therapy. Modern Medicine. 2019;26(1):1-4.
Tinelli V, Cabrini L, Fominskiy E, et al. High flow nasal cannula oxygen vs. conventional oxygen therapy and noninvasive ventilation in emergency department patients: A systematic review and meta-analysis. J Emerg Med. 2019;57(3):322-8.
Wang K, Zhao W, Li J, Shu W, Duan J. The experience of high-flow nasal cannula in hospitalized patients with 2019 novel coronavirus-infected pneumonia in two hospitals of Chongqing, China. Ann Intensive Care. 2020;10(1):37.
Whittle JS, Pavlov I, Sacchetti AD, Atwood C, Rosenberg MS. Respiratory support for adult patients with COVID-19 [published online ahead of print April 13, 2020]. J Am Coll Emerg Physicians Open. 2020. ncbi.nlm.nih.gov/pmc/articles/PMC7228246/














4 Comments.
Very relevant information. I forwarded to all my ICU staff as well as managers for step-down units and Med/surg
I LOVED the information in this article and will be sure to discuss it with colleagues and share it with other nurses who do not belong to ANA and regularly get this caliber information in a timely fashion. I always try to impress on all my colleagues the importance of staying abreast with the latest clinical developments and research. They must stay on top of the information on their practice area. Knowledge is power. Professional development is key!
Very helpful
Very brief and concise.